The Gut-Autoimmunity Loop: How a Leaky Gut May Be Driving Your Autoimmune Symptoms
When your immune system attacks your thyroid, the culprit might be hiding in your gut
The Story No One Told You
Let me tell you something that changed how I think about autoimmune disease: your gut is not just digesting food. It’s training your immune system. And when that gut barrier breaks down, all hell can break loose, including your immune system mistakenly attacking your own thyroid.
If you’re dealing with Hashimoto’s thyroiditis (or suspect you might be) alongside IBS symptoms, this article is for you. I’m going to walk you through the science of what’s actually happening, why these two conditions love to travel together, and what you can actually do about it.
What Is “Leaky Gut” Really?
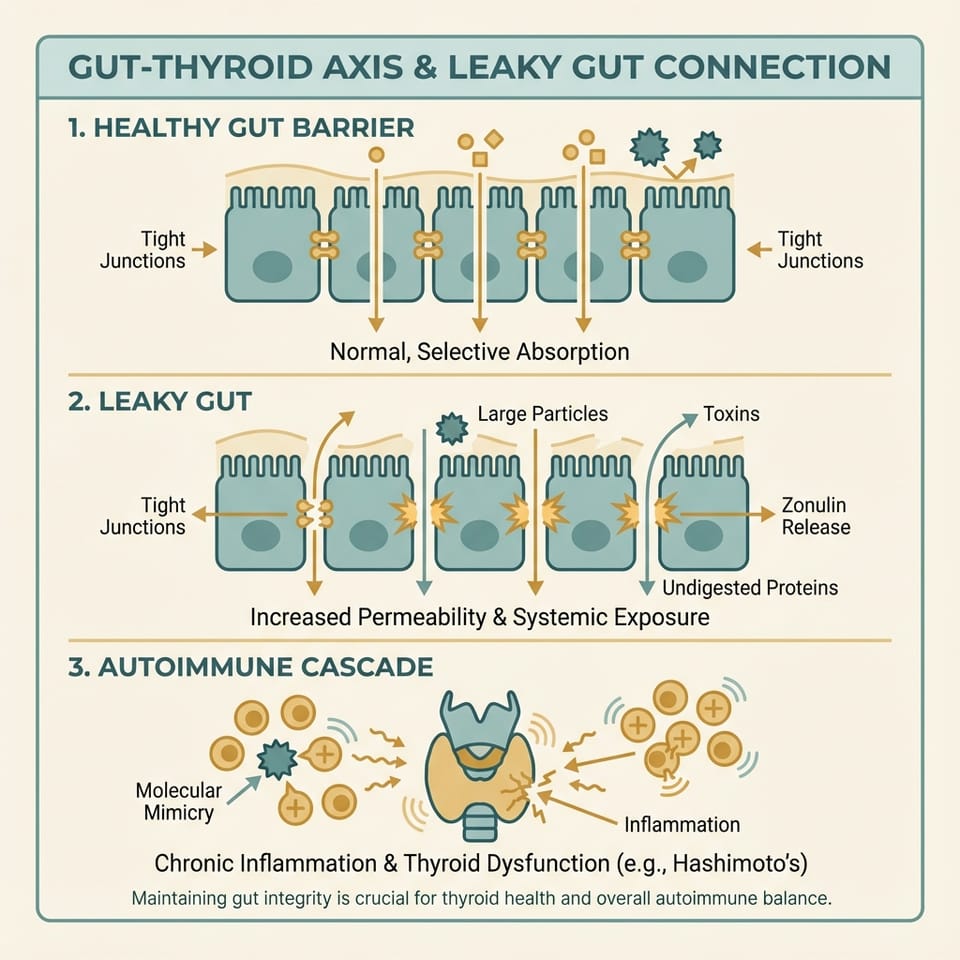
Before we dive deep, let’s demystify this term. “Leaky gut” (or increased intestinal permeability) isn’t pseudoscience, it’s a measurable phenomenon where the tight junctions between intestinal cells loosen, allowing substances that should stay in the gut to slip into the bloodstream.
Here’s how it works:
Your intestinal lining is held together by proteins called tight junctions (ZO-1, occludin, claudins). These act like gatekeepers, deciding what gets absorbed and what stays out. When these junctions weaken, the “gate” opens too wide.
The key player in this drama? Zonulin.
Zonulin is a protein that directly regulates tight junction permeability. When it’s elevated, those junctions loosen. And research has shown that patients with Hashimoto’s thyroiditis have significantly elevated zonulin levels compared to healthy controls (30.92 ng/mL vs 19.01 ng/mL, p = 0.002).[^1][^2]
In other words: people with autoimmune thyroid disease have measurably leakier guts.
The Trilateral Nexus: Gut, Immune System, and Thyroid
Here’s where it gets fascinating. Researchers have identified what they call the “trilateral nexus” connecting three systems:
- Gut Microbiome: The trillions of bacteria living in your intestines
- Immune System: Your body’s defense network
- Endocrine System: Including your thyroid gland
These three systems are in constant communication. When one goes haywire, the others feel it.
How Dysbiosis Drives the Problem
In Hashimoto’s patients, researchers consistently find a distinct microbial signature:[^4][^5][^6]
| What’s Decreased | What’s Increased |
|---|---|
| Faecalibacterium (butyrate producer) | Bacteroides |
| Bifidobacterium (immune regulator) | Phascolarctobacterium |
Why does this matter? Those decreased bacteria produce butyrate, a short-chain fatty acid that literally feeds your gut lining cells and helps maintain tight junctions. When butyrate drops, barrier integrity suffers.
The increased bacteria? They produce more lipopolysaccharide (LPS), an endotoxin that, when it leaks through the compromised barrier, triggers systemic inflammation.
The Diarrheal Microbiome: A Window Into Barrier Breakdown
A fascinating 2025 study revealed something striking about how gut microbes can directly damage your intestinal barrier, even without the bacteria themselves being present.[^EV]
Researchers isolated extracellular vesicles (EVs), tiny messenger packets released by gut bacteria from people with diarrheal conditions. When they introduced these EVs into healthy mice, something alarming happened:
- The mice developed intestinal barrier dysfunction
- Tight junction proteins (ZO-1, occludin) were disrupted
- Pro-inflammatory macrophages flooded the gut
The mechanism? These EVs carried a specific microRNA called miR-125b that hijacks the NF-κB inflammatory pathway, forcing immune cells into an inflammatory state.
What does this mean for you? It suggests that even the “exhaust fumes” from dysbiotic bacteria (not just the bacteria themselves) can perpetuate a leaky gut cycle. Addressing the underlying microbial imbalance isn’t just about killing bad bugs; it’s about changing the entire ecosystem.
Molecular Mimicry: When Your Immune System Gets Confused
Here’s where autoimmunity enters the picture. Your immune system is designed to attack foreign invaders. But what happens when those invaders look suspiciously similar to your own tissues?
This is called molecular mimicry, and research has identified several examples relevant to thyroid autoimmunity:[^5][^10]
| Microbe | Thyroid Risk |
|---|---|
| Helicobacter pylori (CagA protein) | Shares sequences with thyroid peroxidase (TPO) |
| Campylobacter jejuni | 35% identity with thyroglobulin |
| Yersinia enterocolitica | Cross-reacts with TSH receptor |
| Certain Bifidobacterium and Lactobacillus strains | Possess peptides that can bind TPO antibodies |
When these microbial proteins leak through a compromised gut barrier, your immune system mounts an attack. But because these proteins resemble thyroid tissue, the immune response spills over, and suddenly your own thyroid is in the crosshairs.
The SIBO Connection: Why IBS and Hashimoto’s Love Each Other
If you have IBS and Hashimoto’s, there’s a very common bridge between them: Small Intestinal Bacterial Overgrowth (SIBO).
Here’s the vicious cycle:
- Hypothyroidism slows gut motility → Slow-moving contents allow bacteria to overgrow in the small intestine.
- SIBO ferments food prematurely → Producing gas, bloating, and gut distress.
- Bacterial overgrowth increases permeability → More zonulin, more leakiness.
- More inflammation reaches the thyroid → Potentially worsening autoimmunity.
Studies show SIBO affects over 50% of hypothyroid patients.[^13] If you’re struggling with digestive symptoms and thyroid issues, testing for SIBO (with a lactulose or glucose breath test) should be on your radar.
The good news? SIBO is treatable. Rifaximin, a gut-targeted antibiotic, has been shown to normalize breath tests and may even help reduce thyroid autoantibody levels in some patients.[^5]
Biomarkers: How Do You Know If Your Gut Is Leaky?
If you want to assess your gut barrier function, here are the key markers:
Serum Zonulin
This is the most commonly reported marker, correlating with disease severity in Hashimoto’s. But here’s an important caveat: commercial zonulin tests have been shown to cross-react with other proteins (properdin, complement C3), meaning they don’t always measure actual zonulin exclusively.[^17][^18]
Use zonulin as one data point, not the whole picture.
Other Useful Markers
- I-FABP (Intestinal Fatty Acid Binding Protein): Indicates enterocyte damage
- LPS (Lipopolysaccharide): Direct marker of bacterial translocation
- Lactulose/Mannitol Ratio: The functional “gold standard” for measuring permeability
What You Can Actually Do About It
Alright, let’s get practical. If you’re dealing with the gut-thyroid loop, here’s a framework:
Step 1: Rule Out Celiac Disease
Before you try gluten-free anything, get tested for celiac (tTG-IgA + Total IgA). Celiac disease is highly comorbid with Hashimoto’s and shares similar symptoms. Going gluten-free before testing can mask the diagnosis.
Step 2: Test for SIBO
Especially if you have bloating, gas, or alternating bowel habits. A positive breath test gives you a clear treatment target.
Step 3: Address Nutrient Deficiencies
Selenium, Vitamin D, and iron are commonly depleted in Hashimoto’s and directly impact both thyroid and gut function:
- Selenium (200 µg/day): Can reduce anti-TPO antibodies
- Vitamin D: Regulates immune tolerance and barrier integrity
- Iodine: Ensure sufficiency, but avoid excess (>300 µg/day can fuel autoimmunity)
Step 4: Repair the Barrier
- Butyrate supplementation: Sodium butyrate or tributyrin can directly support tight junction repair
- Targeted probiotics: Lactobacillus and Bifidobacterium strains, particularly S. boulardii for barrier support
- L-glutamine: An amino acid that fuels intestinal lining cells
Step 5: Manage Your Diet Strategically
- Short-term Low-FODMAP (4-6 weeks) for symptom relief if IBS is severe
- Transition to high-fiber, diverse diet once symptoms stabilize (Mediterranean-style)
- Gluten-free trial may help some Hashimoto’s patients, but evidence is mixed outside of celiac
